UMAEÂ Â IMSS CD OB. SON
ENFERMEDAD POR REFLUJO GASTROESOFAGICO Y HERNIA HIATAL
Radiology: Volume 243: Number 2—May 2007
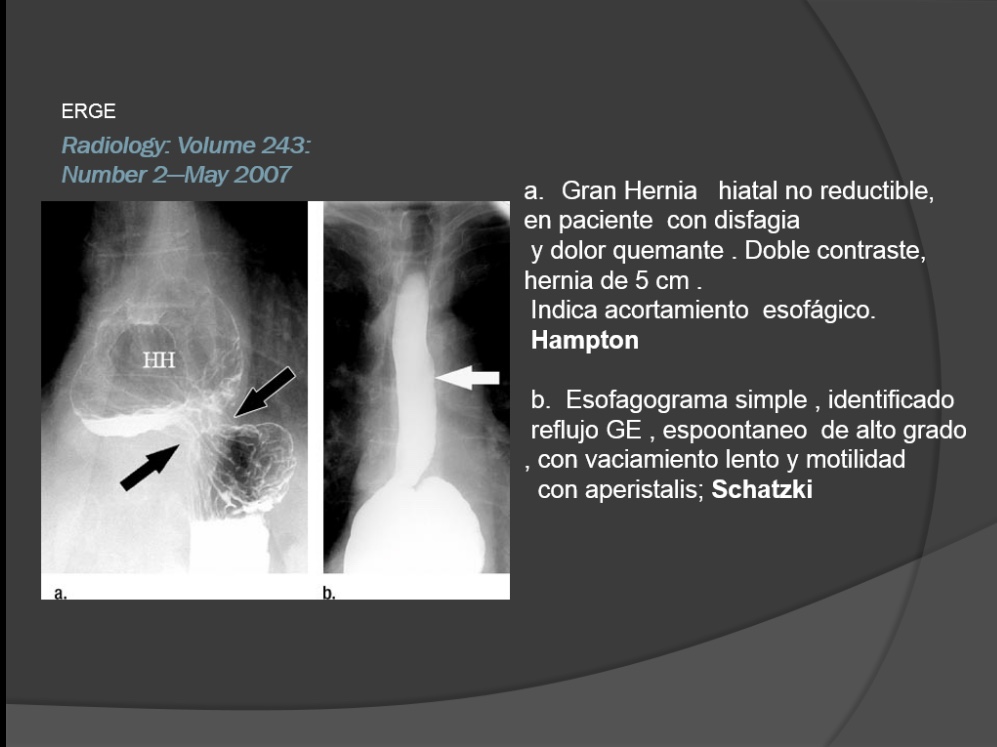
ERGE
[embeddoc url=»https://godieboy.com/wp-content/uploads/2018/06/ERGE-Y-HH.ppt» download=»all» viewer=»microsoft»]
Radiology: Volume 243: Number 2—May 2007
ERGE
Radiology: Volume 243: Number 2—May 2007

ERGE
Radiology: Volume 243: Number 2—May 2007
Objetivo de el esofagograma en ERGE:
Presencia de hernia hiatal o reflujo GE .
–morfologia de secuelas de esofagitis por reflujo , estenosis pepticas,esofago de Barret y adenocarcinoma
ERGEÂ COMPLICACIONES
Radiology: Volume 243: Number 2—May 2007
žThe purpose of barium studies in patients
žwith reflux symptoms is not simply to
ždocument the presence of a hiatal hernia
žor gastroesophageal reflux but to detect
žthe morphologic sequelae of reflux, including reflux esophagitis, peptic strictures,
žBarrett esophagus, and esophageal
žadenocarcinoma.
ERGEÂ COMPLICACIONES
La esofagitis  por reflujo es la enfermedad inflamatoria
Mas comun que involucra al esofago.
El esofago en fase de doble contraste ha demostrado tener una sensibilidad de aproximada de 90% para la detection de  esofagitis por reflujo , debido a la capacidade demostrar anormalidades de la mucosa no evidente en fase simple
.
Most cases that are missed
occur in patients with milder forms of
esophagitis, which manifest at endoscopy
as mucosal erythema and friability.
Most cases that are missed
occur in patients with milder forms of
esophagitis, which manifest at endoscopy
as mucosal erythema and friability.
The single most common sign of reflux
esophagitis on double-contrast esophagrams
is a finely nodular or granular appearance
with poorly defined radiolucencies
that fade peripherally due to edema
and inflammation of the mucosa (Fig 3)
(6,7).
The single most common sign of reflux
esophagitis on double-contrast esophagrams
is a finely nodular or granular appearance
with poorly defined radiolucencies
that fade peripherally due to edema
and inflammation of the mucosa (Fig 3)
(6,7).
This nodularity or granularity almost
always extends proximally from the
gastroesophageal junction as a continuous
area of disease.
This nodularity or granularity almost
always extends proximally from the
gastroesophageal junction as a continuous
area of disease.
.
Barium studies may also reveal shallow
ulcers and erosions in the distal esophagus.
The ulcers can have a punctate, linear,
or stellate configuration and are often
associated with a surrounding halo of
edematous mucosa, radiating folds, or
sacculation of the adjacent wall (Fig 4)
(8).
ESOFAGOGRAMAÂ TECNICA
.
Barium studies may also reveal shallow
ulcers and erosions in the distal esophagus.
The ulcers can have a punctate, linear,
or stellate configuration and are often
associated with a surrounding halo of
edematous mucosa, radiating folds, or
sacculation of the adjacent wall (Fig 4)
(8).
[embeddoc url=»https://godieboy.com/wp-content/uploads/2018/06/ENFERMEDAD-POR-REFLUJO-GASTROESOFAGICO-Y-HERNIA-HIATAL.ppt» download=»all» viewer=»microsoft»]
ESOFAGOGRAMAÂ TECNICA
ERGE
Some patients have a solitary ulcer at
or near the gastroesophageal junction,
often on the posterior wall of the distal
esophagus, presumably as a result of prolonged
exposure to refluxed acid that
pools posteriorly when patients sleep in
the supine position (9).
Radiology: Volume 243: Number 2—May 2007
ERGE
Some patients have a solitary ulcer at
or near the gastroesophageal junction,
often on the posterior wall of the distal
esophagus, presumably as a result of prolonged
exposure to refluxed acid that
pools posteriorly when patients sleep in
the supine position (9).
Radiology: Volume 243: Number 2—May 2007
ERGE
Other patients have more widespread ulceration of the distal third or half of the thoracic esophagus,but this ulceration always extends proximally from the gastroesophageal junction.
 Thus, the presence of ulcers
that are confined to the upper or middle
parts of the esophagus should suggest another
cause for the patient’s disease.
ESOFAGO DE BARRET
Barrett esophagus is characterized by progressive columnar metaplasia of the distal esophagus caused by chronic gastroesophageal reflux and reflux esophagitis.
Barrett esophagus is thought to develop in about 10% of all patients with reflux esophagitis (16).
Double-contrast esophagrams can be used to classify, on
the basis of specific radiologic criteria,patients with reflux symptoms as being at high, moderate, or low risk for Barrett
esophagus (17).
ERGEÂ Â Â COMPLICACIONES
ESOFAGO DE BARRET
Patients are classified at high risk when a barium study reveals a midesophageal stricture (Fig 10) or ulcer or a reticular pattern of the mucosa (usually associated with a hiatal hernia
and/or gastroesophageal reflux) (17).
In such cases, endoscopy and biopsy should
be performed to help obtain a definitive
diagnosis.
Radiology: Volume 243: Number 2—May 2007
ESOFAGO DE BARRET
Although a reticular mucosal
pattern has been found in only 5%–10%
of all patients with Barrett esophagus
(18,19), this finding has been recognized
as a highly specific sign of Barrett esophagus,
particularly if the pattern is adjacent
to the distal aspect of a midesophageal stricture (see Fig 10) (18).
Radiology: Volume 243: Number 2—May 2007
ESOFAGO DE BARRET
The reticular pattern is characterized by tiny barium-filled grooves or crevices resembling the areae gastricae in the stomach.
Patients are classified at moderate risk
for Barrett esophagus when a barium study
reveals esophagitis or peptic strictures in
the distal esophagus (17).
These radiographic findings reflect chronic inflammatory disease and scarring; the decision to perform endoscopy in this group should be based on the severity of symptoms, the age, and the overall health of the patient.
ESOFAGO DE BARRET
Finally, patients are classified at low
risk for Barrett esophagus when barium
studies reveal no structural abnormalities
(regardless of the presence or absence of reflux or a hiatal hernia).
žThe majority of patients are found to be in the low-risk category, and the prevalence of Barrett esophagus is so small in this group that such individuals can be treated empirically for their reflux symptoms without the need for endoscopy (17).
ESOFAGITISÂ INFECCIOSA
CANDIDA
HERPETICA
CITOMEGALAVIRUS
ESOFAGITIS INDUCIDA POR DROGAS
Tetracycline and doxycycline are the two
agents most commonly responsible for
drug-induced esophagitis in the United
States, but other causative agents include
potassium chloride, quinidine, aspirin or
other nonsteroidal antiinflammatory
drugs, and alendronate sodium (33–35).
Affected individuals typically ingest the
medication with little or no water immediately
before going to bed. The capsule
or pill then usually becomes lodged in
the midesophagus, where it is compressed
by the adjacent aortic arch or left
main bronchus.
Prolonged contact of the
esophageal mucosa with these medications
presumably causes an irritant contact
esophagitis. Affected individuals
may present with severe odynophagia,
but marked clinical improvement usually
occurs after withdrawal of the offending
agent.
The radiographic findings in drug-induced
esophagitis depend on the nature
of the offending medication. Tetracycline
and doxycycline are associated with
the development of small shallow ulcers
in the upper or middle part of the esophagus
and are indistinguishable from
those in herpes esophagitis
(Fig 16)
(36,37). Because of their superficial nature,
these ulcers almost always heal
without scarring or strictures. In contrast,
potassium chloride, quinidine, and nonsteroidal
antiinflammatory drugs may
cause more severe esophageal injury leading
to the development of larger ulcers
and possible stricture formation (38–40).
Alendronate sodium (an inhibitor of os
osteoclast–
mediated bone resorption, used
to prevent osteoporosis in postmenopausal
women) may cause severe esophagitis
with extensive ulceration and strictures
that are usually confined to the distal
esophagus (41).
ESOFAGITIS INDUCIDA POR RADIACION
A radiation dose of 5000 cGy or more to
the mediastinum may cause severe injury
to the esophagus. Acute radiationinduced
esophagitis usually occurs 2–4
weeks after the initiation of radiation
therapy (42).
The mucosa typically has
a granular appearance because of edema
and inflammation of the irradiated segment
(42). Ulceration and decreased luminal
distensibility are other frequent
findings (42). The extent of disease conforms
to the margins of the radiation
portal.
Most cases of acute radiation
esophagitis are self-limited, but some
patients may have progressive dysphagia
due to the development of radiation
strictures 4–8 months after completion
of radiation therapy (43). Such strictures
typically appear as smooth tapered
areas of concentric narrowing
within a preexisting radiation portal
(Fig 17).
ENFERMEDAD POR REFLUJO GE
ENFERMEDAD POR REFLUJO GE
Figure 8. Upright LPO spot image from double-
contrast esophagography shows short ringlike
peptic stricture (white arrow) in distal
esophagus above a hiatal hernia (black arrows).
Although this stricture could be mistaken for a
Schatzki ring, it has a longer vertical height
than does a true Schatzki ring.
[embeddoc url=»https://godieboy.com/wp-content/uploads/2018/06/ENFERMEDAD-POR-REFLUJO-GASTROESOFAGICO-Y-HERNIA-HIATAL.ppt» download=»all» viewer=»google»]